Decide to improve your quality of life and call the doctor specializing in angiology IN TIJUANA
Diseases we treat
Angiology and vascular surgery is a specialty of medicine that is responsible for studying and treating diseases of the circulation. It is a medical-surgical specialty, that is, it treats diseases with both medications and surgery when the patient needs it.

All diseases that affect the veins and arteries with the exception of the arteries of the heart and those of the skull, since these are treated by the cardiologist and the neurosurgeon respectively.
The most frequent diseases are: Venous, Varicose veins in all its degrees, venous thromboembolism disease that includes (deep vein thrombosis, pulmonary thromboembolism and post-thrombotic syndrome), varicose ulcers, venous injuries from weapons, surgical complications, hemangiomas and venous malformations.
Angiology and Vascular Surgery
- What are the diseases that an angiologist and vascular surgeon treat? What does an angiologist and vascular surgeon treat?
Arterial Diseases: Chronic arterial insufficiency, acute arterial insufficiency, arterial thromboembolism, arterial aneurysms, aorta and peripheral arteries, vasospastic diseases such as Raynaud's disease, Buerger's disease, etc. Arterial injuries from weapons, or from surgical complications, carotid body tumor (glomus or paragangliomas), carotid disease.
Other diseases: Diabetic foot, chronic wounds, lymphedema.
Patients with renal failure who need vascular access for Hemodialysis such as an arteriovenous fistula or placement of a central venous catheter, patients with cancer who need central venous access such as a reservoir catheter for chemotherapy.
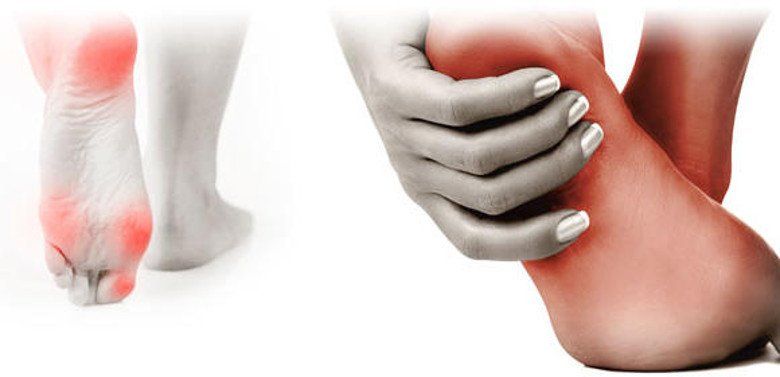
Diabetic foot is a devastating complication of diabetes mellitus, caused by nerve degeneration, occlusion of blood vessels associated with infection and gangrene.

Diabetes mellitus is the main cause of lower extremity loss. 80% of amputations began with an injury that went unnoticed and in most cases could have been avoided. When faced with a foot injury, if you have diabetes, time is money, get treatment as soon as possible and avoid fatal complications.
Diabetic foot
To treat any foot injury in patients suffering from diabetes, what must first be ensured is circulation. If there is no circulation, any treatment is fruitless. Every patient who suffers from diabetes before being amputated should be evaluated by an angiologist and vascular surgeon.
• Pain or fatigue when walking.
• Changes in color or temperature in the skin.
• Dry.
• Ulcers.
• Calluses on the sole of the foot.
• Areas of low sensitivity.
• Immobility in the joints.
• Alterations in the way you walk or balance.
• Cuts, scrapes, blisters, or anything that affects the integrity of the foot.
• Ingrown, thick, infected nails, etc.
Veins are blood vessels that carry blood back to the heart after nourishing the body's organs. From the heart it passes to the lungs to be oxygenated and again sent to the entire body.

This cycle, which is repeated incessantly, has to overcome different obstacles (especially the blood that returns from the feet to the heart). The first obstacle is the force of gravity and the second is the hydrostatic pressure (that is, the blood below must push the blood from above). For this blood return to be carried out properly, there must be integrity in the venous wall and valves. When any of these mechanisms fail, blood returns with difficulty to the heart and can stagnate in the veins, causing dilation, tortuosity (snaking appearance of the veins), edema or swelling.
Chronic Venous Disease or Varicose Veins
In the early stage it only has aesthetic repercussions with the appearance of varicose veins, creating an unpleasant appearance on the legs. Afterwards, pain, cramps, heaviness and fatigue may appear and in the advanced stage there may be complications such as lipodermatosclerosis (indurated and stained skin), bleeding (varicorrhagia), clot formation (varicothrombosis) and ulcers that can be disabling, also affecting family and social life. and emotional of the patient. This condition is commonly known as chronic venous disease, varicose syndrome or varicose veins. The causes of this are: Predisposing factors: Heredity and deep vein thrombosis. Triggering factors: Standing or sitting without moving for a long time, multiple pregnancies, blows or injuries, high doses of female hormones (estrogens), flat feet and exposure to high temperatures.
Aggravating factors: Obesity, sedentary lifestyle and diabetes.
Laser varicose vein surgery
Currently more than 90% of varicose veins can be eliminated in the vast majority of patients who suffer from them. Request a valuation consultation with us and we will help you solve it.
What are the causes and symptoms of thrombosis?
For blood to fulfill its function, it must remain in a liquid state and for this to be the case, there must be a balance between procoagulant and anticoagulant factors. When this balance is altered, thrombosis (thrombophilia) or the opposite, hemorrhage (hemophilia) may occur.

90% of DVT cases occur in the lower extremities, most frequently on the left, and the signs and symptoms are:
Pain, increase in volume, increase in perimeter in the affected limb, color change at the site of thrombosis and edema.
Deep venous thrombosis
We are all at risk of suffering from thrombosis, but if you have one or more of the following history, the risk of developing it increases:
*History of thrombosis in the family.
*History of thrombophilia in the family.
*Suffering from a collagen disease (Rheumatoid arthritis, Scleroderma, Lupus, among others).
*Pregnancy (not all pregnant women experience it).
*Suffering from cancer.
*Obesity.
*Age over 40 years (In certain circumstances).
*Orthopedic surgery (Hip or knee).
*Long trips (more than 4 hours or more than 5000 km) by any means of transport. (Economy class syndrome).
*Prolonged prostration (being in bed for a long time).
*Multiple fractures.
*Immobilization (Use of splint or cast).
*Central venous catheter.
*If you use oral contraceptives or hormone replacement therapy.
*If you already suffered thrombosis, you can present it again.
Diabetic neuropathy
Diabetic neuropathy is a type of nerve damage that can occur if you have diabetes. High blood glucose can damage nerves throughout the body. Diabetic neuropathy most commonly affects the nerves in the legs and feet.
Depending on which nerves are affected, symptoms of diabetic neuropathy include pain and numbness in the legs, feet, and hands. It can also cause problems in the digestive system, urinary tract, blood vessels and heart. For some people, symptoms are mild. However, in other cases, diabetic neuropathy can be quite painful and disabling.
Peripheral neuropathy
This type of neuropathy may also be called distal symmetric peripheral neuropathy. It is the most common type of diabetic neuropathy. It affects the feet and legs first, followed by the hands and arms. The signs and symptoms of peripheral neuropathy usually worsen at night. Among them are the following:
- Numbness and reduced ability to feel pain or perceive temperature changes Tingling or burning sensations Cramps or shooting pains Muscle weakness Extreme sensitivity to touch (for some people, even contact with sheets can be painful) Serious foot problems, such as ulcers, infections, and bone and joint damage
When should you consult a doctor?
Call your healthcare provider to make an appointment if:
- You have an infected or non-healing cut or sore on your foot You have burning, tingling, weakness, or pain in your hands or feet that interferes with your daily activities or sleep You notice changes in digestion, urination, or sexual activity You experience dizziness and fainting
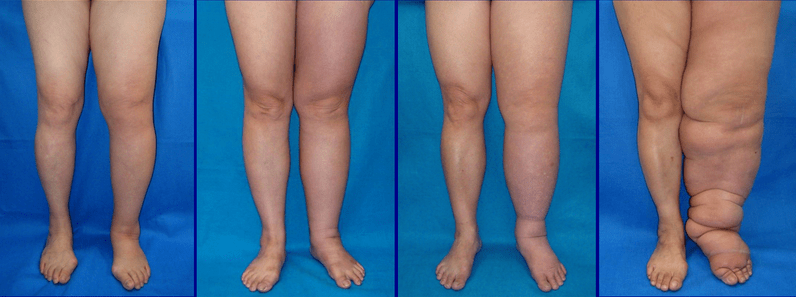
Signs and symptoms of lymphedema include:
- Swelling of all or part of the arm or leg, including the fingers and toesFeeling of heaviness or tightnessLimited range of motionRecurring infectionsHardening and thickening of the skin (fibrosis)
When should you see a doctor
Make an appointment with your doctor if you notice persistent swelling in your arms or legs. If you have already been diagnosed with lymphedema, see your doctor if there is a sudden and drastic increase in the size of the affected limb.
Lymphedema
Complications
Complications of lymphedema may include:
- Skin infections (cellulitis). The trapped fluid creates a favorable terrain for the development of germs, and the slightest injury to the arm or leg can be an entry point for infection. The affected skin looks swollen and red, and is often painful to touch and feels hot. Your doctor may prescribe antibiotics so you have them on hand and can start taking them right away. Septicemia. Untreated cellulite can spread to the bloodstream and trigger septicemia, a life-threatening condition that occurs when the body's response to an infection causes damage to its own tissues. Septicemia requires emergency medical treatment.Drainage through the skin. With severe swelling, lymph fluid can drain through small breaks in the skin or cause blistering.Skin changes. In some people with very severe lymphedema, the skin on the affected limb may thicken and harden, looking like elephant skin.Cancer. A rare form of soft tissue cancer can develop as a result of more severe cases of lymphedema that are not treated.
Vascular Access for Hemodialysis
Dialysis and hemodialysis
End-stage renal failure is treated with dialysis. This procedure removes waste from the blood when the kidneys can no longer do their job.
There are different types of kidney dialysis. This practice focuses on hemodialysis.
What is vascular access?
A vascular access is an opening made in the skin and blood vessel during a short operation. When you have dialysis, your blood flows through the opening into the hemodialysis machine. Once your blood has been filtered in the machine, it flows back through the port in your body.
What is hemodialysis?
The main function of your kidneys is to remove toxins and extra fluid from the blood. If waste products accumulate in the body, it can be dangerous and even cause death.
Hemodialysis can:
- Remove extra salt, water, and waste products so they don't build up in your body Maintain safe levels of minerals and vitamins in your body Help control blood pressure Help make red blood cells
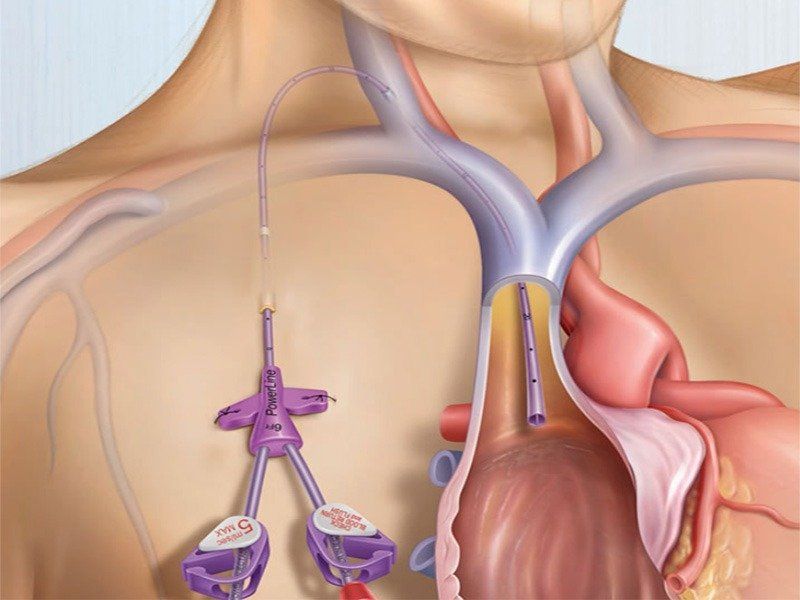
When to call the doctor
- Bleeding from the vascular access site Signs of infection, such as redness, swelling, pain, tenderness, warmth, or pus around the site A fever of more than 100.3°F (38.0°C) Flow (fremitus) in the graft or fistula decreases or does not decrease feel at allThe arm where the catheter was placed swells and the hand on that side feels coldYour hand becomes cold, numb, or weak
Risks and complications
As with any procedure, peripheral vascular intervention involves certain risks and complications that may include the following:
- Allergic reaction to contrast medium. Bleeding or infection at the puncture site. Recurrent narrowing of the artery.
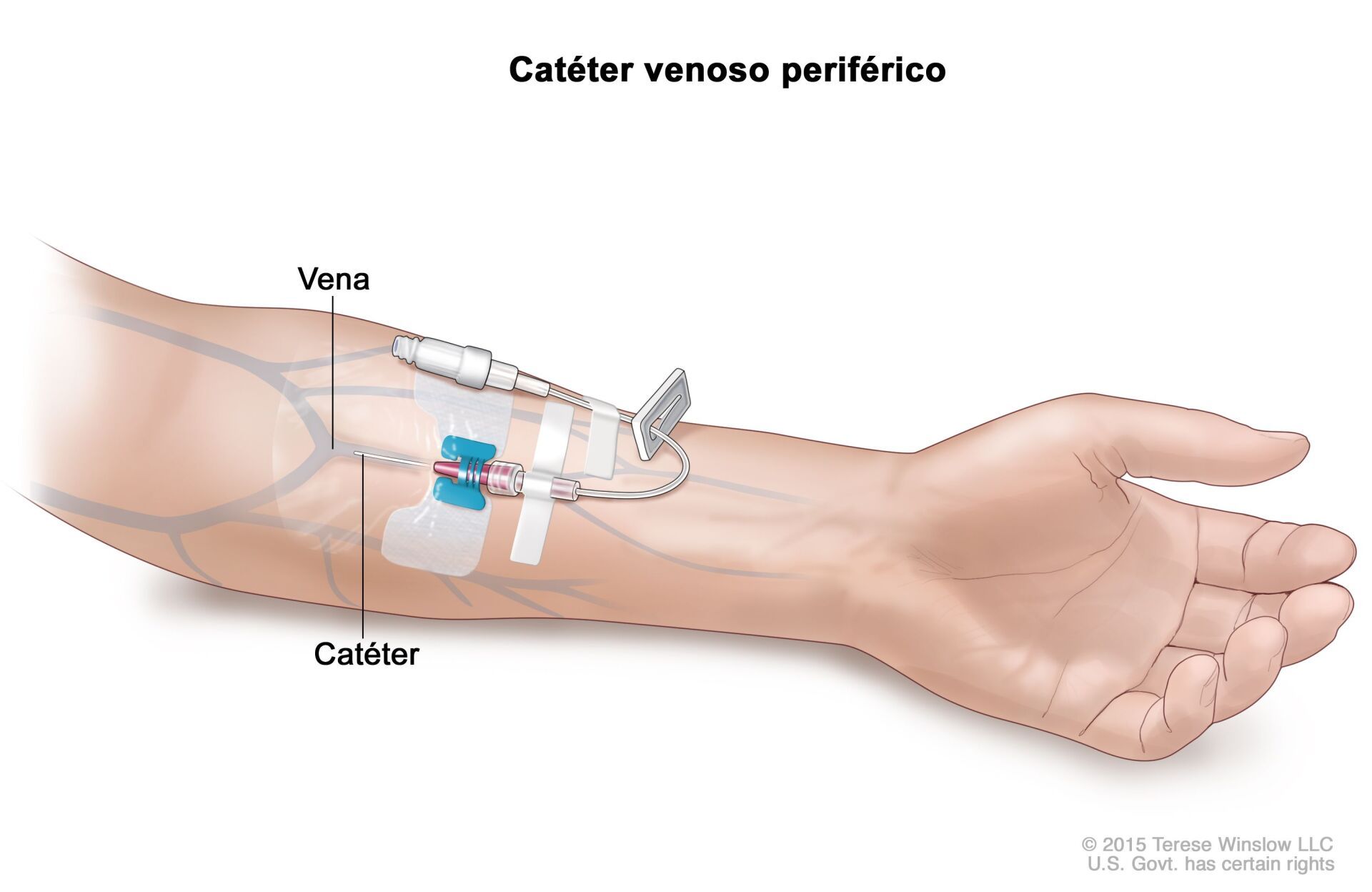
Peripheral Vascular Catheterization
When patients suffer from hardening of the arteries or atherosclerosis, their arteries are partially blocked by a substance called plaque. When these blockages occur in the legs or arms, they are called peripheral artery disease.
In most patients, intravenous fluid and medication needs can be met with a percutaneous peripheral venous catheter. If blind percutaneous placement is difficult, ultrasound guidance usually achieves successful insertion. Rarely, a venous view can be used when percutaneous catheter insertion is not feasible. Typical sites of venous cannulation are the cephalic vein in the arm and the saphenous vein in the ankle. However, venous transection is rarely necessary due to the widespread use of peripherally inserted central catheters (PICC) and intraosseous lines in adults and children.
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Slide title
Write your caption hereButton
Cardiovascular diseases are the third cause of death in Mexico.
Among the most frequent conditions we find chronic venous disease known as varicose veins, varicose ulcer, deep vein thrombosis, chronic arterial insufficiency, acute arterial insufficiency and diabetic foot.
LOCATION
Dr. Gus | Angiologist
Francisco Javier Mina 1415, Mex-Chino Building Zona Urbana Rio 22010 Tijuana, BC
Clinic Hours (By Appointment)
- Mon - Tue
- -
- Wednesday
- Closed
- Thu - Fri
- -
- Saturday
- -
- Sunday
- Closed





